
Flexibility and strength in the feet are essential for ballet dancers to achieve graceful movements and prevent injuries. Toe tapping is a simple yet effective exercise where dancers gently tap their toes on the floor to warm up the foot muscles and improve control. Resistance band exercises helping to build foot and ankle strength, while enhancing flexibility. Foot circles, performed by extending the leg and slowly rotating the foot in each direction, promote better range of motion and joint stability. Additionally, ankle rolls are another key stretch that involves gently rolling the ankles to loosen up the joints and prepare them for demanding routines. If you have incurred a foot or ankle injury during ballet, it is suggested that you contact a podiatrist for appropriate treatment and suggestions about additional effective foot stretches.
Why Stretching Is Important for Your Feet
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Joe Mathew George DPM, FACFAS from Illinois. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Stretching the muscles in the foot is an important part in any physical activity. Feet that are tight can lead to less flexibility and make you more prone to injury. One of the most common forms of foot pain, plantar fasciitis, can be stretched out to help ease the pain. Stretching can not only ease pain from plantar fasciitis but also prevent it as well. However, it is important to see a podiatrist first to determine if stretching is right for you. Podiatrists can also recommend other ways to stretch your feet. Once you know whether stretching is right for you, here are some excellent stretches you can do.
- Using a foam roller or any cylindrical object (a water bottle or soda can will do), roll the object under your foot back and forth. You should also exert pressure on the object. Be sure to do this to both feet for a minute. Do this exercise three times each.
- Similar to the previous exercise, take a ball, such as a tennis ball, and roll it under your foot while seated and exert pressure on it.
- Grab a resistance band or towel and take a seat. If you are using a towel, fold it length wise. Next put either one between the ball of your foot and heel and pull with both hands on each side towards you. Hold this for 15 seconds and then switch feet. Do this three times for each foot.
- Finally hold your big toe while crossing one leg over the other. Pull the toe towards you and hold for 15 seconds. Once again do this three times per foot.
It is best to go easy when first stretching your foot and work your way up. If your foot starts hurting, stop exercising to ice and rest the foot. It is advised that you then see a podiatrist for help.
If you have any questions, please feel free to contact our offices located in Joliet, Bolingbrook, and Channahon, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
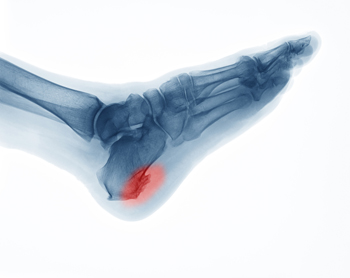
Heel spurs are calcium deposits that build up on the heel bone, often from repetitive strain on the foot’s ligaments and tendons. Several risk factors can increase the likelihood of developing a heel spur. High-impact activities like running, jumping, or dancing may put repeated stress on the heel. Long hours of standing on a hard surface can also contribute. Excess body weight places added pressure on the foot structures and may lead to small tears in the tissue, which may calcify into a spur. Foot structure plays a role as well, as people with flat feet or very high arches may be more prone to heel spurs. Wearing poorly fitting footwear, especially those with minimal arch or heel support, can worsen symptoms. A podiatrist may confirm the diagnosis of heel spurs through an X-ray or MRI scan, and may recommend cortisone injections, a walking boot, or surgery, if symptoms are long-lasting. If you have heel pain, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and appropriate treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Joe Mathew George DPM, FACFAS from Illinois. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Joliet, Bolingbrook, and Channahon, IL . We offer the latest in diagnostic and treatment technology to meet your needs.

Cycling is a great low-impact exercise, but it can still lead to foot pain due to repetitive motion and pressure. Common types of foot pain from cycling include burning sensations, numbness, and sharp pain, often felt in the ball of the foot, arches, or toes. One major cause is wearing cycling shoes that are too tight or lack proper support. Cleat position and pedal pressure can also contribute by placing too much stress on certain areas of the foot. Long rides without adequate breaks or poor bike fit may lead to nerve compression or overuse injuries. Additionally, poor circulation or underlying foot conditions can be aggravated during cycling. If you enjoy cycling but have developed foot pain, it is suggested that you schedule an appointment with a podiatrist who can offer effective relief and treatment solutions.
Ankle and foot injuries are common among athletes and in many sports. They can be caused by several problems and may be potentially serious. If you are feeling pain or think you were injured in a sporting event or when exercising, consult with Joe Mathew George DPM, FACFAS from Illinois. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries
The most common injuries that occur in sporting activities include:
- Achilles Tendonitis
- Achilles Tendon Rupture
- Ankle Sprains
- Broken Foot
- Plantar Fasciitis
- Stress Fractures
- Turf Toe
Symptoms
Symptoms vary depending upon the injury and in some cases, there may be no symptoms at all. However, in most cases, some form of symptom is experienced. Pain, aching, burning, bruising, tenderness, tightness or stiffness, sensation loss, difficulty moving, and swelling are the most common symptoms.
Treatment
Just as symptoms vary depending upon the injury, so do treatment options. A common treatment method is known as the RICE method. This method involves rest, applying ice, compression and elevating the afflicted foot or ankle. If the injury appears to be more serious, surgery might be required, such as arthroscopic or reconstructive surgery. Lastly, rehabilitation or therapy might be needed to gain full functionality in the afflicted area. Any discomfort experienced by an athlete must be evaluated by a licensed, reputable medical professional.
If you have any questions, please feel free to contact our offices located in Joliet, Bolingbrook, and Channahon, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.

